EARLY DETECTION MEANS LIFE
Join Us for our upcoming Thermography Screening Event May 31st
Details below | Share with a bosom buddy | RSVP
Breast cancer is the most common cancer in women, and the risk increases with age. Risk heightens when we have a close relative inflicted by this disease, in addition to women without children, and those who have had their first child after age 30.
However, in this fox trott TOX - ic world, we’re all at risk of developing cancer. Current research indicates that 1 in every 8 women in the US will get breast cancer in their lifetime.
Can we win? I believe WE CAN, and t’s all about awareness and prevention.
Learn more about Thermography and save your spot for this great opportunity - gaining sense of ease and empowerment at the same time.
WHAT IS THERMOGRAPHY?
Thermograms are incredibly powerful and reliable for early cancer detection (and many other health nuances which you’ll see below).
Thermograms can be used for successful diagnosis, treatment, & prognosis. They are completely painless, non-invasive and take less than 15 minutes for a thorough reading.
MAMMOGRAMS VS THERMOGRAPHY
Unlike mammograms, thermograms emit no harmful ionizing radiation. Mammograms are one of the more dangerous medical tools due to the very high amounts of ionizing radiation. Thermograms use infrared technology that is completely safe.
They also do not compress the breast tissue like mammograms. This compression that takes place during mammograms can cause cancer cells to break off create a malignant spread through the bloodstream.
The use of Digital Infrared Imaging is based on the principle that metabolic activity and vascular circulation in both pre-cancerous tissue and the area surrounding a developing breast cancer is almost always higher than in normal breast tissue.
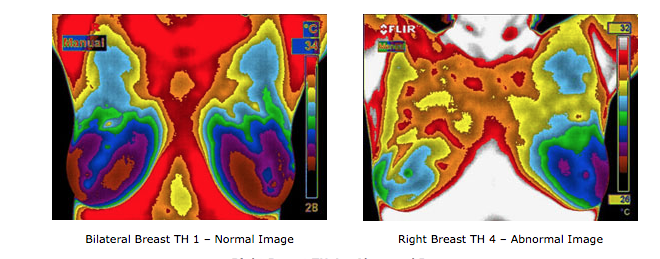
Infrared cameras and sophisticated computers detect, analyze, and produce high-resolution images of temperature variations, and may be among the earliest signs of breast cancer and/or a pre-cancerous state of the breast.
Since the absolute prevention of breast cancer has not become a reality as of yet, efforts must be directed at detecting breast cancer at its earliest stage.
WHAT MAKES DIGITAL INFRARED IMAGING SO UNIQUE
While mammography, ultrasound, MRI, and other structural imaging tools rely primarily on finding the physical tumor, DII is detecting minute variations in normal blood vessel activity and may find thermal signs suggesting a pre-cancerous state of the breast or the presence an early tumor that is not yet large enough to be detected by physical examination, mammography, or other types of structural imaging.
Certain types of cancers will not be detected (approximately 20%) by mammography for various reasons, but some of these cancers can be discovered by DII.
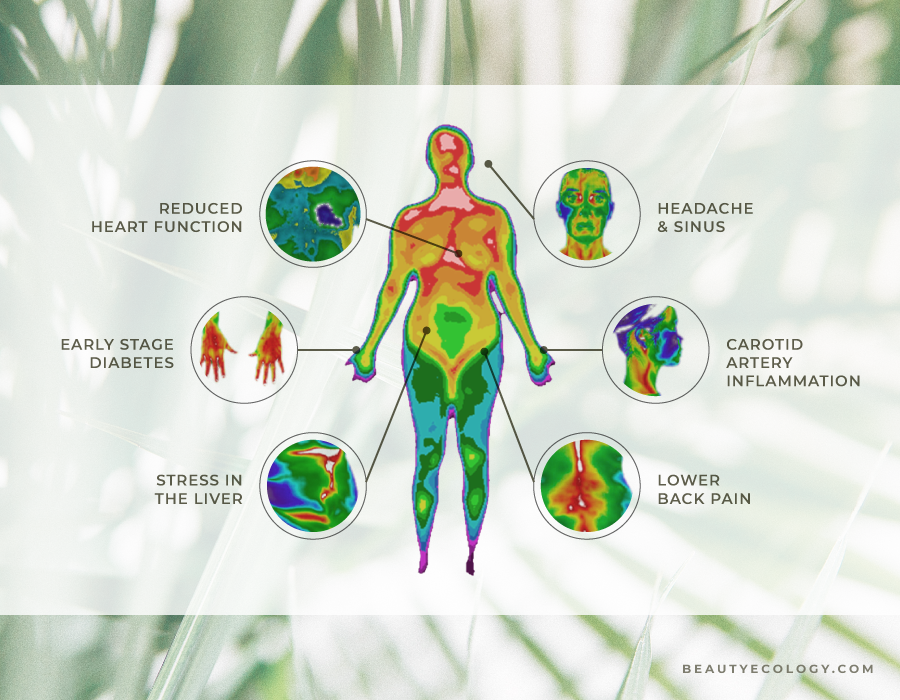
THERMOGRAPHY IMAGE EXAMPLE
WHO REVIEWS YOUR IMAGE?
Rest assured, your image is digitally produced, and interpreted by qualified doctors. Abnormalities or changes in infrared images provide invaluable information. This is particularly true in patients with dense breasts, non-specific physical or mammographic findings, or women with a previous history of breast surgery or radiation.
BETTER TOGETHER? WHEN BREAST THERMOGRAPHY & MAMMOGRAPHY JOIN FORCES
Thermography does not replace mammography and mammography does not replace DII, the tests can greatly complement each other. Since it has been determined that 1 in 8 women will get breast cancer, we must use every means possible to detect cancers when there is the greatest chance for survival. Proper use of breast self-exams, physician exams, DII, and mammography together provide the earliest detection system available to date. If treated in the earliest stages, cure rates greater than 95% are possible.
IT’S NOT JUST ABOUT THE BOOB
OTHER REASONS FOR USING THERMOGRAPHY
Arthritis: Thermography can help you detect early signs of arthritis -- and differentiate between osteoarthritis and more severe forms like rheumatoid. Effective early treatment strategies can then be implemented, before you experience further degeneration.
Neck and Back Pain: Thermal pain patterns ‘light up' white and red hot on a scan in the involved area. You can get relief faster and begin restorative care that more precisely targets the correct area.
Dental Issues: If you have TMJ, gum disease, or an infected tooth, this will show up on a thermal scan as white or red hot.
Sinus Issues & Headaches: Significant heat in your forehead or sinus region revealed on a thermal scan is an indicator that these systems in your body are not functioning properly.
Immune Dysfunction, Fibromyalgia and Chronic Fatigue: The immune system correlates to the T1 andT2 areas of your spine -- high levels of heat in that region can indicate immune dysfunction. On the other hand, chronic fatigue, fibromyalgia, and aching joints are just a few complaints that correlate to cool patterns seen at this area.
Carpal Tunnel Syndrome (CTS): This condition is often misdiagnosed. For instance, you may think you have CTS, yet the scan shows your neck is referring pain from a different affected area. This will help you get the most appropriate treatment.
Digestive Disorders: Irritable bowel syndrome, diverticulitis and Crohn's disease are often visible with thermography. If you're able to address these conditions early on, you'll find that health restoration is much more likely.
Other Conditions: Including bursitis, herniated discs, ligament or muscle tear, lupus, nerve problems, whiplash, stroke screening, cancer, and many, many others.
NOW THAT IS EMPOWERING! IF YOU’RE READY TO GRAB YOUR SAFE SCREENING……
Next steps:
Please email me directly at hello@beautyecology.com - Suggest times best for you from 2pm to 8pm.
I will reply with available times for you to confirm.
I will send you all Q/A information and how to prep for your thermogram.
Cheers! All set. Please bring the forms when you come. You’re an incredible woman for taking your ownership of your health!
FDA Disclaimer
The information on this website has not been evaluated by the Food & Drug Administration or any other medical body. We do not aim to diagnose, treat, cure or prevent any illness or disease. Information is shared for educational purposes only. You must consult your doctor before acting on any content on this website, especially if you are pregnant, nursing, taking medication, or have a medical condition.